Inform your specialist prior to the Gastroscopy if you have any of the following:
- Allergy to any medication or anaesthetic
- Diabetes
- Heart or lung problems including pacemakers and artificial heart valves
- Artificial joint replacements
- Are pregnant or breast-feeding
- Take blood-thinning medications (these may need to be stopped prior to the procedure)
- Take iron supplements (these need to stop one week before the colonoscopy). Iron can produce black stool which can coat the lining of the bowel, reducing visibility.
- Unless otherwise instructed, continue taking any regularly prescribed medication.

What happens on the day of your gastroscopy?
After arrival to the Cambridge Specialist Centre you will be admitted by a nurse and you will see the specialist performing the procedure to discuss and sign a consent form. You will then be asked to change into a hospital gown.
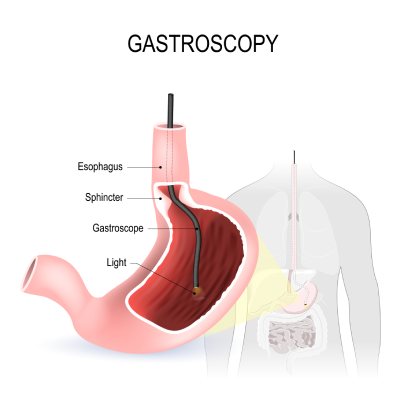
The gastroscopy will be performed in a fully equipped examination room in our endoscopy suite. In the examination room the back of your throat will be sprayed with a local anaesthetic spray which has a bitter taste and makes your tongue and the back of the throat feel numb. Intravenous medication (a sedative and pain medication) will be offered. These medications will relax you, and possibly make you fall asleep. You will be assisted and observed by two endoscopy nurses throughout the procedure who will monitor your heart rate and oxygen levels. In most instances you will be lying on your left side and a mouth guard will be inserted to protect your teeth.
Your specialist will insert the gastroscope through your mouth and gently advance down the oesophagus and stomach into the duodenum. The gastroscope does not interfere with your breathing. Tissue samples may be taken with tiny biopsy forceps inserted through the scope and photographs may be taken. The procedure generally takes about 10 minutes but could be longer particularly if you require any endoscopic treatment during the test.

What happens after a gastroscopy
After your gastroscopy you will be wheeled into the recovery room where you will rest to allow the sedation to wear off. If you have received intravenous sedation you will be required to be in the recovery room for at least one hour after the procedure. When you wake up your specialist will discuss your examination results with you and a written summary will be given to you for your reference.
A light snack will be served before you leave the Cambridge Specialist Centre. You are able to return to your normal diet following discharge.
If you have received sedation you must have someone to take you home after the test and stay with you, as you will be drowsy. This generally wears off after a few hours. You will not be allowed to drive a car, operate machinery or make any important decisions for 24 hours as your judgement and reflexes may be impaired. The sedation may also affect your ability to recollect details of the gastroscopy. You should stay off work the day of your procedure but can resume normal activities the following day.
Any tissue samples are sent to the pathology department for examination under a microscope. These results will be sent to your specialist and GP within 5-7 days. A typed report of your procedure will also be sent to your GP. You may be asked to make a follow-up appointment with your specialist to discuss your results.
Safety and Risks
A gastroscopy is generally a very safe and simple test. Complications are very rare but may include:
- Bleeding and/ or perforation (tearing) of upper gastrointestinal tract may occur, especially if procedures such as biopsy, polypectomy or dilatation are performed.
- Adverse reaction to sedative medication, causing breathing problems or low blood pressure (4 out of 10,000 tests).
- Allergic reaction to the throat spray.
Contact Us
Booking a consultation
Get in touch today with one of our team and we’ll arrange a time that suits you to see one of our specialists.

 07 444 4600
07 444 4600 email us
email us